Topical Steroids 101
What does “topical” mean?
Prescription instructions for any medication include the route in which the medication is meant to be administered. Some examples of routes are: oral, inhaled, under the tongue, injected, etc.
The definition of topical is, “a medication that is administered to a particular spot on the outer surface of the body.” Outer surfaces of the body include skin and mucous membranes.
What are Topical Steroids?
Corticosteroids, often known as steroids, are an anti-inflammatory medication prescribed for a wide range of conditions. They are a synthetic, or man-made, version of hormones normally produced by the adrenal glands (two small glands that sit on top of the kidneys).
Steroids mimic natural hormones produced in the body, including glucocorticoids (such as cortisol) and mineralocorticoids (such as aldosterone). Topical steroids vary in structure depending the type of synthetic hormone incorporated, whether alone or combined with other adrenal cortex hormones.
The adrenal hormones of topical steroids are not related to the androgenic hormones of anabolic steroids (often abused by body-builders to increase muscle mass).
Topical steroids can reduce inflammation (redness and swelling), suppress the immune system, and narrow the blood vessels in the skin. Their main purpose is to reduce skin inflammation and irritation.
How do they work?
Topical steroids are absorbed into the cells of the skin. The mechanism of the anti-inflammatory activity of the topical steroids, in general, is unclear. (source: paragraph 12.1 “Mechanism of Action” )
It is believed that topical steroids stop skin cells from producing various inflammation-causing chemicals that are normally released when the skin reacts to allergens or irritation.
These inflammation-causing chemicals, including prostaglandins and leukotrienes, cause blood vessels to widen (vasodilate) and signal other inflammatory substances to arrive. This results in the affected area of skin becoming red, swollen and itchy.
By preventing these inflammatory chemicals from being released in the skin, topical steroids reduce inflammation and relieve related symptoms such as itchiness. Learn more about how corticosteroids work here.
Are Topical Steroids considered safer than steroids that are injected or taken by mouth?
Topical medications are thought to have limited absorption, while medications taken by mouth or injected are considered to have systemic absorption. However, absorption of topical steroids can vary greatly depending on many factors:
- Age – The very young and very old have higher rates of absorption due to thinner skin. Children also have a greater body surface area to weight ratio and are less able to metabolize the drug quickly.
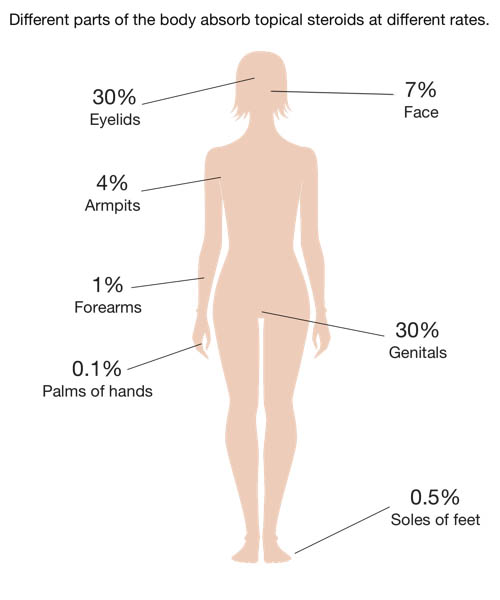
- Thickness of the skin – Thin skin is able to absorb more steroids than thick skin. Skin thickness varies with age and region of the body. Areas of thinner skin include: eyelids, face or genitals. Skin can also become thinner with high potency or long-term steroid use, or both.
- Condition of the skin – Absorption is increased on open, cracked, or raw skin, or skin that has lesions. The type of lesion topical steroids are applied to also play a part in absorption.
- Percentage of the body surface area treated – Treating large areas of the body allows for greater absorption, especially in children where there is a higher ratio of skin surface area to body mass. For instance, topical steroid drug inserts state, “Pediatric patients applying topical corticosteroids to greater than 20% of body surface are at higher risk of HPA axis suppression”(source: Momemtasone furoate cream 0.1% prescription information, paragraph 8.4)
- Time frame used – Usage for longer periods of time, especially without breaks, increases absorption. “Do not use daily TCS [topical corticosteroids] continuously for more than two to four weeks . . . Your provider should strive to help create a safe and effective long-term treatment plan that does not include daily use of TCS, especially on more sensitive areas.” source: National Eczema Association
- Vehicle – Ointments are absorbed more than creams, creams more than lotions, etc.
- Occlusion – Topical steroid-treated areas covered by tight-fitting pajamas or clothes, gauze wraps, bandages, diapers, or any other means of occlusion, increases the level of absorption.
- Site treated – Certain areas of skin absorb more than others, such as areas that rub together (between the thighs or buttocks or under the breasts), as well as the face, genitals, eyelids and underarms (axilla).
- Concurrent use of multiple steroid preparations – Topical corticosteroids can be prescribed by many different practitioners at the same time (General Practitioner, Pediatrician, Allergist, Dermatologist, etc.) without being reconciled by each prescribing physician. Also, many patients are simultaneously prescribed other corticosteroid preparations in addition to topical steroids: oral steroids, inhalers, nebulizers, nasal sprays, eye drops, etc. Using multiple steroids at once, whether over-the-counter or prescription, has a cumulative effect.
What about topical steroid potency? What does potency mean?
Potency is a measure of drug activity expressed in terms of the amount required to produce an effect of given intensity. A highly potent drug evokes a larger response at low concentrations, while a drug of lower potency evokes a small response at low concentrations.
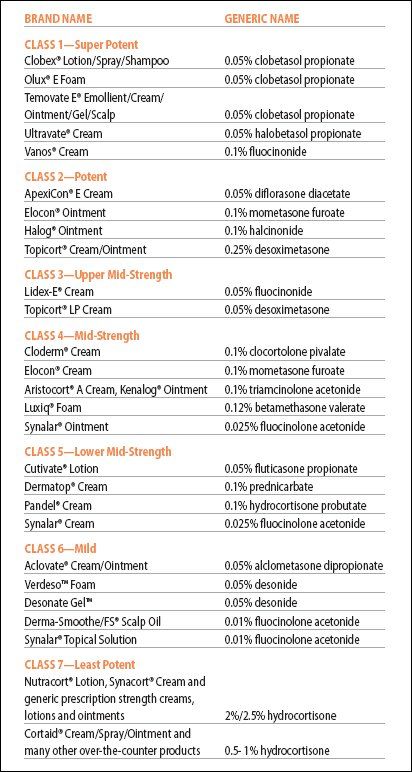
Topical steroids are classified by potency ranging from Class 1 “Super Potent” to Class 7 “Least Potent” topical steroids. Class 1 topical steroids such as Clobetasol propionate 0.05% or Betamethasone dipropionate 0.05%, are up to 600 times as potent as Class 7 Hydrocortisone.
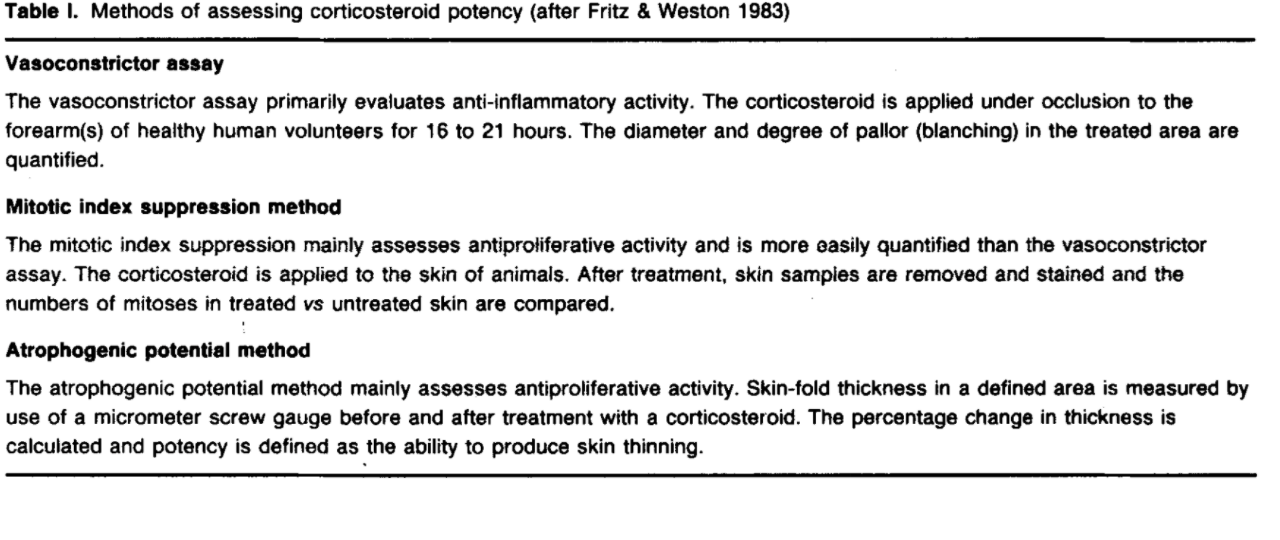
Potency is determined by various techniques. During the vasoconstrictor assay the application of topical corticosteroid blanches the skin by constricting dermal blood vessels, and this level of blanching is evaluated to determine the potency of the steroid. The mitotic index suppression method assesses anti-proliferative activity of skin cells that have been treated with topical steroids, resulting in less mitosis or cell division. The atrophogenic potential assay shows the ability of a compound to cause skin atrophy by measuring thickness of the skin before and after treatment with corticosteroids. (See table in sidebar.)
The age of the patient is a major consideration for determining the appropriate class and potency level. See sidebar for more information on topical steroid potency and age guidelines.
What are some of the side effects of Topical Steroids?
Side effects of topical steroid use fall into two categories: Systemic side effects and local side effects.
Systemic side effects 0ccur in tissues distant from the site of contact. Topical steroids become absorbed into the bloodstream and affect other systems of the body, such as the eyes, endocrine, immune, skeletal, and gastrointestinal systems, in addition to the integumentary system.
Local side effects are those that adversely impact the skin at the site of application.
Systemic side effects occur in tissues distant from the site of contact. Topical steroids become absorbed into the bloodstream and affect other systems of the body, such as the eyes, endocrine, immune, skeletal, and gastrointestinal systems, in addition to the integumentary system.
- Cushing syndrome: A condition that occurs from exposure to high cortisol levels for an extended period of time (such as long term exposure to cortisol present in topical steroids).
- Hypothalamic-Pituitary-Adrenal (HPA) axis suppression: the HPA axis is a highly interdependent endocrine unit which monitors various hormone levels and responds by releasing appropriate stimulatory or inhibitory hormones. Depressed HPA activity is characterized by decreased levels of cortisol production, and can occur due to the supplementation of synthetic cortisol in topical steroid preparations. Impairment may be confined solely to adrenals or extend to the hypothalamus and pituitary glands and their respective hormones.
- Hyperglycemia/Type 2 diabetes: Corticosteroids increase insulin resistance thus allowing blood glucose levels to rise and remain higher.
- Hypertension: elevated blood pressure
- Hypertrichosis/hirsutism: excessive hair growth, or male patterned hair growth in women.
- Ocular changes: cataracts, glaucoma, occular hypertension
- Osteoporosis: bones become weak or brittle
- Linear Growth Retardation: suppression of the pituitary gland (due to HPA axis suppression) leads to stunted growth in children.
- Topical Steroid Withdrawal Syndrome: also known as Topical Steroid Addiction (TSA) or Red Skin Syndrome (RSS), can arise from topical steroids being applied to the skin for medical or cosmetic purposes. Characterized by red, itchy, stinging, burning skin which appears after ceasing topical steroid treatments, or even between treatments. As topical steroid therapy is withdrawn to effectively treat TSWS, multiple local and systemic symptoms emerge and eventually resolve over a long period of time.
Source: Meyler’s Side Effects of Endocrine and Metabolic Drugs, Jeffrey K. Aronson, Elsevier 2009, page 93.
View a full list of local and systemic side effects here.
Please keep in mind that ITSAN does not provide medical advice. We ask that you always consult your doctor for questions, or when making decisions about your medical treatment.
Structural classification
Topical steroids are categorized by structural class: Different structural classes of steroids will cross-react with each other to cause hypersensitivity reactions.
| Class A: | hydrocortisone type |
| Class B: | triamcinolone acetonide type |
| Class C: | betamethasone type |
| Class D1: | betamethasone dipropionate type |
| Class D2: | methylprednisolone aceponate type |
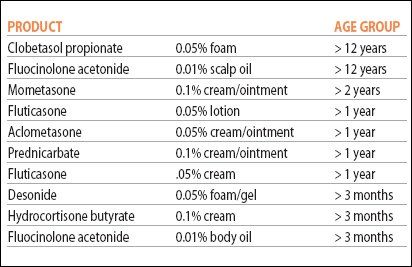
Age guidelines
Age guidelines for topical steroids (source NEA). Click to enlarge:
Absorption
Different parts of the body absorb topical steroids at different rates.
Source: Walden, Pamela BSN, RN, OCN, Hardaway, Ann MSN, RN, Petrus, Brenda BSN, RN, OCN “Med Check: Not just skin deep: Topical steroids”, Nursing Made Incredibly Easy! July/August 2011, Volume :9 Number 4, page 49 – 50.
Potency classification
Common topical steroids by potency class (source NEA, see also psoriasis.org). Click to enlarge:
How Potency is Established
Click to enlarge:
Source: Goa, K.L. Clinical Pharmacology and Pharmacokinetic Properties of Topically Applied Corticosteroids. Drugs 36, 51–61 (1988). https://doi.org/10.2165/00003495-198800365-00011